Myofascial pain syndrome (MPS) manifests as discomfort due to taut bands and trigger points (TP) affecting muscles, tendons, ligaments, and fascia. This prevalent condition affects approximately 12% of the population, notably prevalent among individuals aged 30-50.
Diagnosis relies on identifying trigger points—hyperirritable spots within muscle fibers’ taut bands, often confirmed through physical examination and patient history. Occasionally, diagnostic imaging or electromyography is utilized to exclude alternative conditions.
How does auricular vagus nerve stimulation work to alleviate pain in MPS patients?
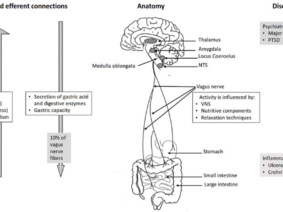
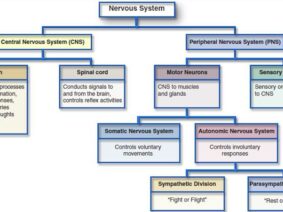
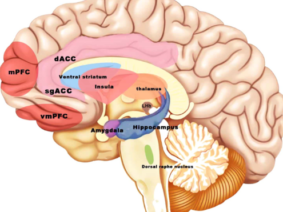
The pursuit of innovative treatments for MPS led to the investigation of auricular vagus nerve stimulation (VNS). Auricular vagus nerve stimulation (VNS) is a non-invasive method that involves the stimulation of the auricular branch of the vagus nerve, which is located in the ear. The vagus nerve is known to play a role in pain modulation, and VNS has been shown to activate the descending pain inhibitory pathway. In a recent study by Ünal, S., Karagözoğlu Coşkunsu, D., Hatık, S. H., & Özden, A. V. (2022), VNS was applied from both ears noninvasively to avoid possible asymmetric effects of unilateral stimulation. Tragus and concha regions were stimulated concomitantly to increase the affected auricular vagus nerve fibers. The study found that the addition of VNS to ischemic compression and stretching exercises resulted in significant improvements in pain severity, trigger point sensitivity, grip strength, quality of life, and autonomic functions in MPS patients.
Analyzing Study Results: Pain Severity, Quality of Life, and Autonomic Function Improvements
The study found that both the VNS group and the control group showed significant improvements in pain severity, trigger point sensitivity, and grip strength after 10 sessions of treatment. However, the VNS group showed statistically higher improvements in pain severity, trigger point sensitivity, and grip strength compared to the control group. In terms of quality of life, the control group showed significant improvements in all parameters of the Short Form-36 (SF-36) scale, while the VNS group showed significant improvements in physical function, social functionality, and pain parameters. In terms of autonomic function, a statistically significant improvement was found in orthostatic intolerance, secretomotor, and pupillomotor subscales of the Composite Autonomic Symptom Scale-31 (Compass-31) scale in the VNS group following the treatment, while no significant difference was observed in the control group.
Potential of VNS Beyond MPS: Treatment for Other Chronic Pain Conditions
Emerging evidence in the literature suggests its potential efficacy in addressing neuropathic pain, fibromyalgia, and chronic migraine. Nevertheless, further dedicated investigations are requisite to validate these preliminary findings and understand the optimal parameters for VNS treatment across diverse chronic pain conditions.
The study by Ünal et al. marks a significant stride toward understanding the augmentation of conventional MPS treatments through VNS integration. Its outcomes signify a potential avenue for improving patient outcomes and merit deeper exploration to harness the full spectrum of VNS efficacy in mitigating the complex realm of chronic pain conditions.
References: