Inflammatory bowel disease (IBD) is a chronic condition characterized by disrupted gut homeostasis, chronic inflammation, and ulcerative lesions. Current treatments for IBD often fall short in providing long-term remission, leading to the exploration of novel therapeutic approaches. The vagus nerve (VN) has emerged as a potential target due to its role in the pathogenesis of IBD, involving decreased parasympathetic activity and impaired communication between the enteric and central nervous systems. Vagus nerve stimulation (VNS) has shown promise in various inflammatory disorders, including IBD, by suppressing the production of inflammatory cytokines. This review explores the therapeutic potential of VNS in IBD, particularly focusing on noninvasive techniques such as transcutaneous auricular VNS.
Inflammatory bowel disease (IBD) is a chronic inflammatory condition of the gastrointestinal tract, encompassing Crohn’s disease and ulcerative colitis. Despite advancements in treatment, many patients experience disease recurrence and struggle with long-term remission. This has prompted the investigation of alternative therapies, including vagus nerve stimulation (VNS), which targets the dysfunctional neuroimmune axis implicated in IBD pathogenesis.
Vagus Nerve Dysfunction in IBD
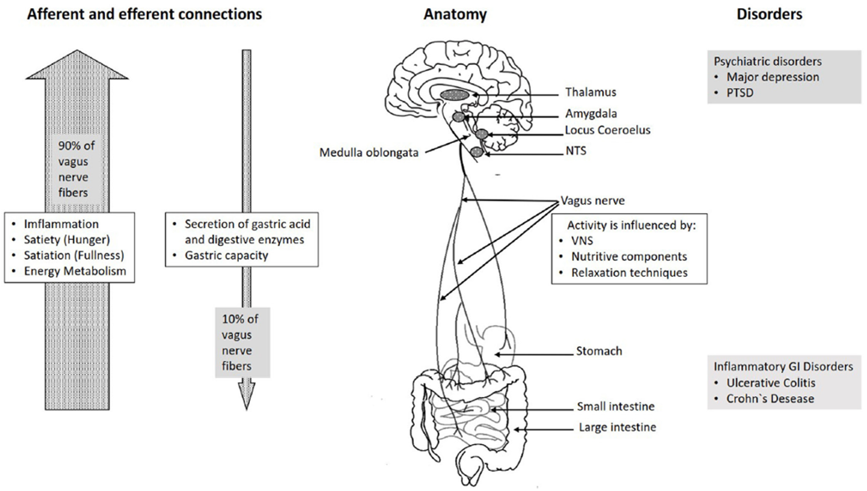
Diminished parasympathetic activity, particularly within the vagus nerve, plays a significant role in the pathophysiology of IBD. Studies have demonstrated decreased vagal tone in IBD patients, contributing to dysregulated immune responses and chronic inflammation. The brain-gut axis, mediated by the vagus nerve, regulates gastrointestinal homeostasis and immune function, highlighting its potential as a therapeutic target in IBD management.
Mechanisms of Vagus Nerve Stimulation
Vagus nerve stimulation modulates the inflammatory response through several mechanisms. Stimulation of the efferent vagus nerve fibers activates the cholinergic anti-inflammatory pathway, leading to inhibition of pro-inflammatory cytokine production by immune cells. Additionally, VNS enhances the release of anti-inflammatory mediators, promoting resolution of inflammation and tissue repair.
Clinical Evidence and Therapeutic Potential
Preclinical and clinical studies have demonstrated the efficacy of VNS in ameliorating disease activity and promoting mucosal healing in IBD models and patients. Noninvasive techniques such as transcutaneous auricular VNS offer a promising alternative to invasive VNS devices, providing targeted stimulation with minimal side effects. Moreover, the potential synergistic effects of VNS with conventional IBD therapies warrant further investigation.
References
[1] Fatemeh Hesampour, Charles N Bernstein, Jean-Eric Ghia, Brain-Gut Axis: Invasive and Noninvasive Vagus Nerve Stimulation, Limitations, and Potential Therapeutic Approaches, Inflammatory Bowel Diseases, Volume 30, Issue 3, March 2024, Pages 482–495, https://doi.org/10.1093/ibd/izad211
[5] McAllen, R. M., Shafton, A. D., Bratton, B. O., Trevaks, D., & Furness, J. B. (2018). Calibration of thresholds for functional engagement of vagal A, B and C fiber groups in vivo. Bioelectronic Medicine, 4(1), 3.