Investigating the Role of the Autonomic Nervous System in Sleep-Induced Depression: Implications for Transcutaneous Auricular Vagus Nerve Stimulation
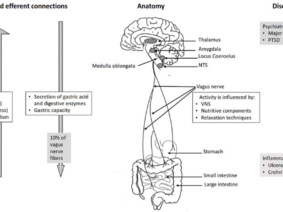
A recent article delves into the intricate relationship between insufficient sleep and depression, with a particular emphasis on the involvement of the autonomic nervous system (ANS) in mediating this connection. Drawing from both population-based research and animal experimentation, the study aims to elucidate the effects of preventive transcutaneous auricular vagus nerve stimulation (taVNS) on autonomic nerves within a chronic sleep deprivation mouse model.
Notable findings reveal a significant correlation between sleep duration, heart rate variability (RMSSD), and depression scores, thus indicating a compelling link between sleep insufficiency and depression mediated by ANS dysfunction. Furthermore, the research showcases taVNS as a potential therapeutic avenue by demonstrating its ability to ameliorate the adverse effects of sleep restriction on RMSSD. These findings underscore the promising role of taVNS in alleviating depression associated with insufficient sleep and offer valuable insights into the underlying mechanisms of sleep-induced depression.
Sleep-Induced Depression
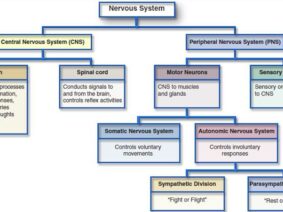
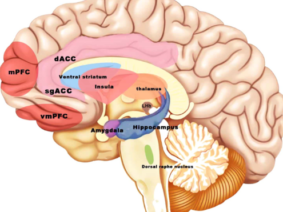
Depression remains a prevalent and debilitating mental health condition, often intricately intertwined with sleep disturbances. While the relationship between sleep and depression is well-documented, the underlying mechanisms linking these phenomena remain incompletely understood. Recent research suggests that the autonomic nervous system (ANS) may serve as a crucial mediator in this complex interplay, offering a promising avenue for therapeutic intervention. In light of this, the present study seeks to investigate the role of the ANS in sleep-induced depression and explore the therapeutic potential of transcutaneous auricular vagus nerve stimulation (taVNS) as a preventive measure.
Methods:
The study employs a multifaceted approach, combining population-based research with animal experimentation to comprehensively examine the relationship between sleep, depression, and ANS function. Population-based analyses are conducted to assess the correlation between sleep duration, heart rate variability (RMSSD), and depression scores in a diverse sample population. Additionally, a chronic sleep deprivation mouse model is established to investigate the effects of preventive taVNS on autonomic nerves and behavioral outcomes.
Results:
Key findings from the population-based research reveal a significant association between sleep duration, RMSSD, and depression scores, indicating a potential causal link between sleep insufficiency and depression mediated by ANS dysfunction. In parallel, animal experiments demonstrate that chronic sleep deprivation induces ANS impairment, as evidenced by reduced RMSSD. However, preventive taVNS interventions effectively mitigate these negative effects, restoring RMSSD levels and attenuating depressive symptoms in sleep-deprived mice.
The findings of this study underscore the intricate interplay between sleep, depression, and ANS function, highlighting the potential role of taVNS as a therapeutic intervention for sleep-induced depression. By elucidating the mechanisms underlying this relationship, the research contributes valuable insights to the field of mental health and paves the way for novel treatment strategies aimed at improving emotional well-being in individuals with sleep disturbances.
In conclusion, this study sheds light on the role of the autonomic nervous system in mediating the connection between insufficient sleep and depression. The findings underscore the therapeutic potential of transcutaneous auricular vagus nerve stimulation (taVNS) as a preventive measure for depression associated with sleep disturbances. Moving forward, further research in this area is warranted to refine our understanding of the underlying mechanisms and optimize the efficacy of taVNS as a therapeutic intervention for sleep-induced depression.
References