The gastrointestinal tract, a complex network of nerves and muscles, plays a central role in the body’s digestive processes. Recent advances in medical science have unlocked a promising avenue for treating gastrointestinal disorders through bioelectric neuromodulation. This groundbreaking technique utilizes non-invasive vagus nerve stimulation to alleviate a range of gastrointestinal problems. The potential of this therapy stems from the gastrointestinal tract’s extensive connections with the central nervous system, which can be harnessed to improve patient outcomes.
The Gastrointestinal Conundrum
Gastrointestinal disorders, including inflammatory bowel disease (IBD), obesity, nausea, and gastroparesis, have posed significant challenges for medical professionals. Traditional treatment approaches have shown variable success, leaving patients searching for more effective and less invasive alternatives. This is where bioelectric neuromodulation enters the spotlight.
A Gateway to Gastrointestinal Solutions
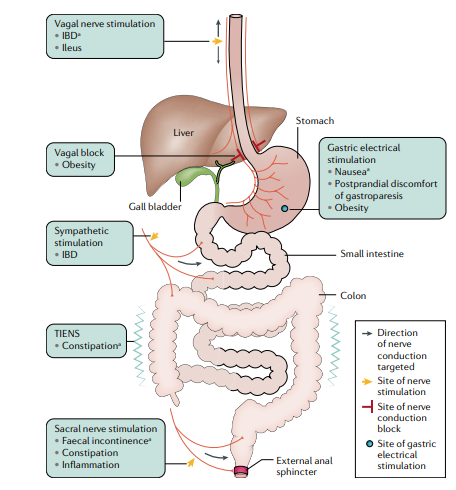
While sacral nerve stimulation has found success in addressing fecal incontinence, the potential applications of non-invasive vagus nerve stimulation are far-reaching. The digestive system’s intricate nerve connections provide a surgical gateway to explore and manipulate the neurological mechanisms behind gastrointestinal disorders. Research has shown that nerves are instrumental in modulating inflammation in the intestine, a vital clue to the puzzle of gastrointestinal health.
The Power of Vagal Nerve Stimulation
One remarkable revelation in this field is the anti-inflammatory potential of vagal nerve stimulation. Recent trials have shown positive effects of this approach in specific cases, notably in some Crohn’s disease patients. By stimulating the vagus nerve, it’s possible to counteract the inflammation responsible for many gastrointestinal disorders, opening the door to more effective treatments.
Beyond Inflammation: Tackling Obesity
High-frequency current pulses applied to the vagus nerve offer a unique approach to address obesity. By blocking signaling from the stomach to the brain, appetite can be regulated. However, outcomes have been mixed, highlighting the need for further research to optimize this approach.
Expanding the Horizon: Disorders and Applications
Bioelectric neuromodulation is not limited to specific disorders; it has been explored for a variety of conditions, including postoperative ileus, gastroparesis symptoms, and constipation. Both animal models and clinical trials have provided valuable insights, although consistent success remains a challenge.
The Path to Enhanced Clinical Success
To maximize the clinical success of bioelectric neuromodulation therapy, researchers are working on several fronts. First and foremost is a deeper understanding of the targeted nerve pathways within the gastrointestinal system. By pinpointing these pathways, medical professionals can tailor stimulation protocols to specific disorders, enhancing efficacy. Moreover, patient selection is a crucial aspect of treatment optimization, ensuring that the right candidates benefit most from this groundbreaking therapy.
Conclusion
Non-invasive vagus nerve stimulation represents a promising frontier in gastrointestinal medicine. As bioelectric neuromodulation technology continues to evolve, it offers renewed hope for individuals grappling with a range of gastrointestinal issues. By understanding the intricate neural pathways, their functions, and refining stimulation protocols, we are edging closer to unlocking the full potential of this transformative therapy. With ongoing research and clinical trials, non-invasive vagus nerve stimulation has the potential to revolutionize the treatment of gastrointestinal ailments, providing a brighter future for countless patients.
References:
- Payne, S.C., Furness, J.B. & Stebbing, M.J. Bioelectric neuromodulation for gastrointestinal disorders: effectiveness and mechanisms. Nat Rev Gastroenterol Hepatol 16, 89–105 (2019). https://doi.org/10.1038/s41575-018-0078-6