In recent years, auricular vagus nerve stimulation (aVNS) has gained increasing attention as a potential therapeutic approach for various medical conditions. The vagus nerve, a complex cranial nerve, has long been explored for its therapeutic potential, dating back to early research in the 1960s. One significant milestone was Dr. Jake Zabara’s discovery in 1992, which demonstrated that repetitive stimulation of the vagus nerve in the neck could effectively stop seizures in a canine model. This breakthrough eventually led to the FDA approval of vagus nerve stimulation (VNS) as an anticonvulsant [George et al., 2004].
The auricular branch of the vagus nerve, a more accessible target for non-invasive stimulation, has emerged as an attractive option for modulating vagal activity. However, the field of aVNS has encountered challenges due to conflicting results in early-stage clinical trials for various medical indications [Verma et al., 2021]. In this article, we delve into the mechanisms behind auricular vagus nerve stimulation, shedding light on the factors contributing to these conflicting findings.
The Auricular Vagus Nerve
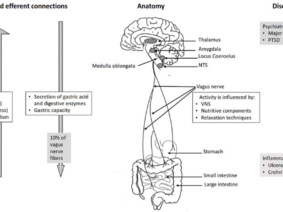
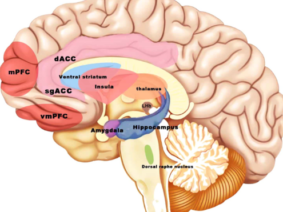
The auricular branch of the vagus nerve runs superficially along the ear, making it an ideal target for non-invasive stimulation techniques. This approach offers the potential to modulate vagal activity, which plays a pivotal role in regulating autonomic functions, including heart rate and inflammation.
Conflicting Results and Bias in aVNS Studies
Recent systematic reviews of randomized controlled trials (RCTs) on aVNS have highlighted a significant challenge—the presence of bias in these studies. The Cochrane Risk of Bias tool was employed to assess the quality of evidence, revealing that a substantial number of aVNS studies were at “some” or “high” risk of bias [Verma et al., 2021]. This bias can make it challenging to interpret the results in a broader context and may explain the inconsistencies observed in clinical trials.
Heart Rate and Heart Rate Variability
One of the key physiological responses to aVNS is the modulation of heart rate. Studies have shown a modest decrease in heart rate during higher stimulation dosages, often surpassing the level of sensory discomfort. However, the findings on heart rate variability, another important parameter reflecting autonomic nervous system activity, have varied between studies. These discrepancies may be attributed to trial design differences, including inappropriate washout periods and diverse methods used to quantify heart rate variability [Verma et al., 2021].
Inflammatory Markers and Pain Management
Emerging evidence suggests that aVNS may have anti-inflammatory effects, as it can reduce both circulating and endotoxin-induced levels of inflammatory markers. Additionally, aVNS has shown promise in ameliorating pathological pain, although its efficacy in managing evoked pain remains uncertain [Verma et al., 2021].
Future Directions and Optimizations
In light of the challenges and conflicting results in aVNS studies, it is imperative to implement improvements in research methodologies and trial designs. Direct measures of local neural target engagement are crucial for optimizing electrode design, placement, and stimulation waveform parameters to enhance on-target engagement while minimizing off-target activation [Verma et al., 2021].
Moreover, consistent evaluation of blinding success in clinical trials is essential, as this was identified as a significant concern in the Cochrane analysis. These measures and improvements are not only applicable to aVNS but also have broader implications for the development of other paresthesia-inducing neuromodulation therapies and their control designs.
Auricular vagus nerve stimulation represents a promising avenue for non-invasive neuromodulation in the treatment of various medical conditions. However, the conflicting results observed in clinical trials underscore the need for rigorous study design, reduction of bias, and direct measures of neural target engagement. As our understanding of the mechanisms behind aVNS continues to evolve, it holds the potential to revolutionize the treatment of conditions ranging from epilepsy to chronic pain and inflammation.
References:
- Verma N, Mudge JD, Kasole M, Chen RC, Blanz SL, Trevathan JK, Lovett EG, Williams JC, Ludwig KA. Auricular Vagus Neuromodulation-A Systematic Review on Quality of Evidence and Clinical Effects. Front Neurosci. 2021 Apr 30;15:664740. doi: 10.3389/fnins.2021.664740. PMID: 33994937; PMCID: PMC8120162.
- George, M. S., Nahas, Z., Bohning, D. E., Mu, Q., Kozel, F. A., Borckhardt, J., & Denslow, S. (2004). Mechanisms of action of vagus nerve stimulation (VNS). Clinical Neuroscience Research, 4(1–2), 71-79. doi: 10.1016/j.cnr.2004.06.006.