Depression, a complex and pervasive mental health condition, is influenced by a myriad of factors ranging from genetics to environmental stressors. Among these influences lies a fascinating link with the autonomic nervous system (ANS), the body’s intricate control system regulating involuntary functions. Understanding the interplay between depression and the ANS sheds light on novel therapeutic avenues and enhances our comprehension of this multifaceted disorder.
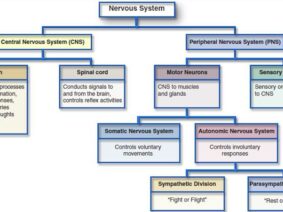
The ANS, comprised of the sympathetic and parasympathetic branches, orchestrates physiological responses to stress and emotions. An imbalance within this system, marked by heightened sympathetic activity and diminished parasympathetic tone, emerges as a significant contributor to depression. This dysregulation disrupts the body’s stress response mechanisms, fostering an environment conducive to depressive symptoms.
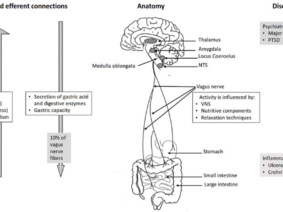
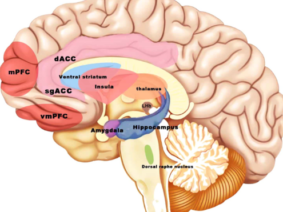
At the heart of this connection lies the vagus nerve, a key player in the parasympathetic branch of the ANS. Research indicates that individuals with depression often exhibit altered vagal tone, as evidenced by reduced heart rate variability (HRV), a marker of autonomic function. The vagus nerve’s role extends beyond basic physiological regulation; it also modulates inflammatory responses, exerting a profound influence on immune function.
Studies suggest that high vagal tone, reflected in elevated parasympathetic parameters, can mitigate inflammation by tempering cytokine production. Inflammatory processes are increasingly implicated in the pathogenesis of depression, with elevated levels of cytokines observed in individuals experiencing depressive episodes. Thus, the dysregulation of the ANS, particularly involving the vagus nerve, contributes to the inflammatory milieu characteristic of depression.
Moreover, the impact of ANS imbalance extends to neurotransmitter function and emotional regulation, further intertwining with depression’s pathophysiology. Heightened sympathetic activity may disrupt neurotransmitter balance, particularly serotonin and norepinephrine, which play pivotal roles in mood regulation. Concurrently, diminished parasympathetic tone impairs emotional resilience, exacerbating susceptibility to depressive symptoms.
Recognizing the bidirectional relationship between depression and ANS dysfunction opens avenues for innovative therapeutic interventions. Interventions targeting ANS modulation, such as biofeedback and Vagus Nerve Stimulation, hold promise in ameliorating depressive symptoms by restoring autonomic balance. Additionally, lifestyle modifications, including stress management techniques and aerobic exercise, offer tangible strategies for enhancing ANS function and mitigating depressive risk.
In conclusion, the intricate interplay between depression and the autonomic nervous system underscores the complexity of this prevalent mental health disorder. ANS imbalance, characterized by heightened sympathetic activity and diminished parasympathetic tone, contributes to dysregulation in stress response mechanisms, inflammation, and emotional regulation, perpetuating the cycle of depression. By elucidating this relationship, we pave the way for targeted interventions that address the physiological underpinnings of depression, ultimately improving treatment outcomes and enhancing quality of life for individuals grappling with this debilitating condition.