Post-Traumatic Stress Disorder (PTSD) is a complex and often debilitating condition that can affect individuals who have experienced trauma. Characterized by chronic feelings of threat and hyperarousal, PTSD can significantly impact a person’s mental and emotional well-being. While various treatments have been explored to alleviate the symptoms of PTSD, recent research has focused on the potential of non-invasive Vagus Nerve Stimulation (tVNS) as a novel approach to improving the lives of those affected by this disorder.
Two groundbreaking studies, Lamb et al. (2017) and Bremner et al. (2021), have provided valuable insights into the effects of tVNS on individuals with PTSD, particularly those with a history of mild traumatic brain injury (mTBI). These studies shed light on the promising prospects of tVNS as an intervention for PTSD management.
Understanding Post-Traumatic Stress Disorder (PTSD)
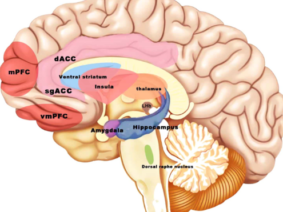
PTSD arises as a result of exposure to traumatic events, leading to a chronic perception of threat and an overactive autonomic nervous system. This overactivity can manifest as emotional dysregulation and chronic disinhibition of limbic structures in the brain. Moreover, military veterans are particularly susceptible to developing PTSD, often due to mTBI, which can affect white matter networks crucial for emotional regulation.
The Potential of tVNS
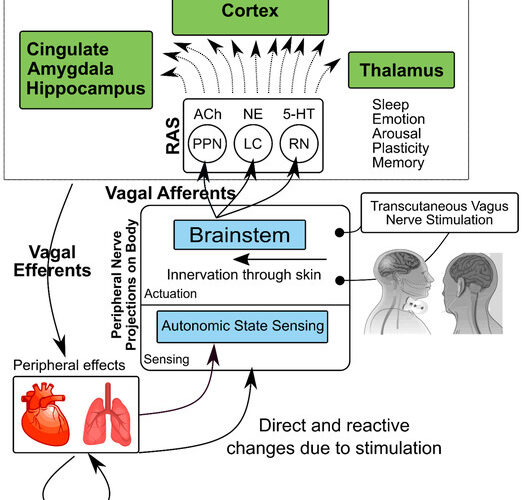
Transcutaneous Vagus Nerve Stimulation (tVNS) presents an intriguing solution to the challenges of managing PTSD. It is a non-invasive, low-risk approach that aims to modulate the functions of the limbic-cortical and peripheral networks involved in the hyperarousal component of PTSD. By targeting these systems, tVNS may provide relief and improve the overall health and well-being of individuals living with PTSD.
Preliminary Findings: tVNS and Improved Vagal Tone
In the study conducted by Lamb et al. (2017), a pilot investigation involving 22 combat veterans with PTSD, the researchers employed tVNS and compared its effects with a sham group. The primary measures included respiratory sinus arrhythmia (high-frequency heart rate variability) and skin conductance changes in response to emotional stimuli. The results were promising. Participants who received tVNS exhibited improved vagal tone and better autonomic responses to stress, indicating that tVNS could modulate the autonomic state and response to stress in this population.
Bremner et al. (2021) expanded on this research by investigating the effects of transcutaneous cervical Vagus Nerve Stimulation (tcVNS) on PTSD symptoms and inflammatory responses to stress. Their study included 20 patients with PTSD who were randomized into active tcVNS or sham stimulation groups. During exposure to personalized traumatic scripts, tcVNS effectively blocked the increase in the inflammatory marker interleukin-6 (IL-6) in PTSD patients.
Over a three-month period, active tcVNS resulted in a significant reduction in PTSD symptoms, particularly hyperarousal symptoms and somatic anxiety. Moreover, open-label tcVNS led to further improvements in patients’ overall clinical condition. These findings suggest that tcVNS not only reduces inflammatory responses to stress but also has a positive impact on PTSD symptoms.
Innovative PTSD Management with tVNS
The studies conducted by Lamb et al. (2017) and Bremner et al. (2021) provide compelling evidence for the potential of non-invasive Vagus Nerve Stimulation as a valuable tool in the management of PTSD. By modulating autonomic responses, reducing inflammatory markers, and alleviating core PTSD symptoms, tVNS and tcVNS offer hope for those living with this debilitating condition.
While further research is needed to confirm and expand upon these findings, the preliminary results are promising. As our understanding of the neurobiological underpinnings of PTSD continues to evolve, innovative treatments like tVNS may play a crucial role in improving the lives of individuals affected by this condition. As researchers continue to explore this field, we can anticipate the development of more targeted and effective interventions for PTSD, ultimately providing a brighter outlook for those on the path to recovery.
References
- J. Douglas Bremner, Matthew T. Wittbrodt, Nil Z. Gurel, MdMobashir H. Shandhi, Asim H. Gazi, Yunshen Jiao, Oleksiy M. Levantsevych, Minxuan Huang, Joy Beckwith, Isaias Herring, Nancy Murrah, Emily G. Driggers, Yi-An Ko, MhmtJamil L. Alkhalaf, Majd Soudan, Lucy Shallenberger, Allison N. Hankus, Jonathon A. Nye, Jeanie Park, Anna Woodbury, Puja K. Mehta, Mark H. Rapaport, Viola Vaccarino, Amit J. Shah, Bradley D. Pearce, Omer T. Inan,
Transcutaneous Cervical Vagal Nerve Stimulation in Patients with Posttraumatic Stress Disorder (PTSD): A Pilot Study of Effects on PTSD Symptoms and Interleukin-6 Response to Stress,Journal of Affective Disorders Reports,Volume 6,2021,100190,ISSN 2666-9153,https://doi.org/10.1016/j.jadr.2021.100190.
(https://www.sciencedirect.com/science/article/pii/S2666915321001165) - Lamb DG, Porges EC, Lewis GF, Williamson JB. Non-invasive Vagal Nerve Stimulation Effects on Hyperarousal and Autonomic State in Patients with Posttraumatic Stress Disorder and History of Mild Traumatic Brain Injury: Preliminary Evidence. Front Med (Lausanne). 2017 Jul 31;4:124. doi: 10.3389/fmed.2017.00124. PMID: 28824913; PMCID: PMC5534856.
- Bremner JD, Gurel NZ, Wittbrodt MT, Shandhi MH, Rapaport MH, Nye JA, Pearce BD, Vaccarino V, Shah AJ, Park J, et al. Application of Noninvasive Vagal Nerve Stimulation to Stress-Related Psychiatric Disorders. Journal of Personalized Medicine. 2020; 10(3):119. https://doi.org/10.3390/jpm10030119